Articles
Article Tools
Stats or Metrics
Article
Original Article
Exp Neurobiol 2024; 33(1): 18-24
Published online February 29, 2024
https://doi.org/10.5607/en23034
© The Korean Society for Brain and Neural Sciences
Exploring Brainstem Structural Abnormalities: Potential Biomarkers for Panic Disorder
Hye-Min Kim1, Chanmi Kang2, Boram Chae1, June Christoph Kang2* and Ho-Kyoung Yoon1*
1Department of Psychiatry, Korea University Ansan Hospital, Ansan 15355,
2Department of Brain and Cognitive Engineering, Korea University, Seoul 02841, Korea
Correspondence to: *To whom correspondence should be addressed.
June Christoph Kang, TEL: 82-2-6401-0199, FAX: 82-2-929-1917
e-mail: cnsla@korea.ac.kr
Ho-Kyoung Yoon, TEL: 82-31-412-5140, FAX: 82-31-412-5144
e-mail: hkhkgogo@korea.ac.kr
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Panic disorder (PD), characterized by recurrent and intense panic attacks, presents a complex interplay between psychological and neurobiological factors. Although the amygdala and hippocampus have been studied extensively in the context of PD, the brainstem’s involvement remains relatively underexplored. This study aims to address this gap by examining structural abnormalities within specific brainstem regions, including the medulla, pons, and midbrain. The study sample population comprised twenty-one adult patients diagnosed with PD and an age-gender-education-matched control group. Utilizing rigorous inclusion and exclusion criteria, confounding factors related to comorbid psychiatric conditions and brain structure abnormalities were minimized. Our findings revealed a significant reduction in medulla volume among PD patients, a finding that persisted even after correcting for individual differences in total intracranial volume. The medulla’s role in cardiovascular regulation and autonomic function, coupled with its involvement in fear responses, underscores its potential significance in the pathophysiology of PD. This study elucidates the medulla’s structural abnormalities as a potential biomarker for PD. Understanding the role of the brainstem in PD could pave the way for more targeted and effective interventions for this condition.
Graphical Abstract
Keywords: Autonomic nervous system, Brain stem, Medulla oblongata, Panic disorder
INTRODUCTION
Panic disorder (PD) is characterized by recurrent, unexpected panic attacks manifesting as sudden and intense fear or discomfort. These episodes often involve autonomic symptoms and cognitive fear-related symptoms [1]. Although several brain regions are believed to be involved in the development of PD, the brainstem plays a critical role [2]. Gorman’s fear network model proposes that the amygdala, hypothalamus, and brainstem collectively contribute to fear responses, forming a network through their connections [3]. Conventionally, the central amygdala’s efferent projections are known to mediate the behavioral and autonomic aspects of conditioned fear [4]. However, when it comes to the generation of panic attacks, the brainstem takes on significant importance. Studies in monkeys conducted using autoradiographic methods have suggested multiple projection pathways from the amygdala to several brainstem nuclei associated with autonomic function [5]. The brainstem’s role as an intermediary between the hypothalamus and autonomic neurons underscores its involvement in the pathophysiology of PD, potentially linked to disturbances in the autonomic nervous system [6]. In response to threats, a two-dimensional defense system is categorized into defensive avoidance and defensive approach. Proximal threats activate the periaqueductal gray (PAG) in the brainstem, creating a panic-freeze response, whereas distal threats engage the limbic system, which is associated with phobia-related responses. Serotonin, norepinephrine, and gamma-aminobutyric acid, among other neurotransmitter systems, are thought to play a role in the pathogenesis of panic and anxiety. In particular, serotonin is pivotal in the pathophysiology, with drugs that enhance serotonergic activity showing promise in alleviating panic symptoms by desensitizing fear networks between the amygdala and brainstem [7, 8]. Research indicates that PD is associated with diminished serotonergic activity in the raphe nuclei, indicating the role of the brainstem’s serotonergic system [9, 10]. Brain imaging techniques have also shown correlations between PD and decreased 5-HT1A receptor availability in the raphe and 5-HT transporter binding within the midbrain raphe [11, 12]. These findings suggest an imbalance in the serotonin system in individuals with PD, with a negative correlation between symptom severity and midbrain 5-HT transporter binding. Similarly, neuroimaging studies have reported associated abnormalities in the brainstem. Neumeister et al. [13] used positron emission tomography (PET) on patients with PD and found a pronounced decrease in 5-HT1A receptor binding within the midbrain raphe in patients, implying a connection between PD and the brainstem. Other research has revealed increased midbrain activity among patients with PD, both before and after exposure to substances such as pentagastrin [14]. A study by Sakai and colleagues showed that cerebral glucose metabolism was characterized by elevated glucose utilization in the midbrain, caudal pons, and medulla of individuals with PD [15]. While research has identified structural anomalies in various brain regions within the fear network in PD, the brainstem’s specific role has not been thoroughly investigated. This study aimed to explore structural abnormalities in specific brainstem regions, including the midbrain, pons, and medulla, using magnetic resonance imaging (MRI), with a focus on their contribution to the pathophysiology of PD while considering potential confounding variables.
MATERIALS AND METHODS
Subjects and procedures
The study sample consisted of twenty-one adult patients with PD, aged 18 to 65, who were recruited from the Department of Psychiatry at the Korea University Anam Hospital. All participants were right-handed, as assessed using Edinburgh Handedness Test [16]. Patients who met the criteria for the diagnosis of PD, as defined by the DSM-IV (Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition), were recruited for participation [17]. For diagnosing psychiatric disorders, the Korean version of the MINI (Mini-International Neuropsychiatric Interview) tool was administered by board-certified psychiatric professionals [18]. The exclusion criteria for patients with PD were as follows: (1) any past or current comorbid psychiatric disorders, such as mood disorders, psychotic disorders, anxiety disorders, substance-related disorders, or personality disorders; (2) intelligence quotient under 80; (3) clinically significant general and/or neurological disease that may influence brain structure on imaging; (4) pregnancy or breastfeeding; and (5) any contraindication to undergoing MRI, such as the presence of a pacemaker. Twenty-one healthy controls matched for age (p=0.487), gender (same numbers), and education level (p=0.283) were recruited via community advertisements. All controls were screened to exclude a history of major psychiatric disorders, ensuring no participant in the healthy control group had psychiatric disorders. Following a thorough explanation of the study, all participants provided written informed consent. The study procedures were approved by the Institutional Review Board of the Korea University Anam Hospital.
Assessment for psychopathology
The intensity of participants’ panic symptoms was assessed using the Panic Disorder Severity Scale (PDSS) [19]. Three different scales were used to assess anxiety symptoms: the Hamilton Anxiety Rating Scale (HAM-A), the Anxiety Sensitivity Index-Revised (ASI-R), and the State-Trait Anxiety Inventory (STAI), comprising both State (STAI-S) and Trait (STAI-T) versions [20-22].
Image acquisition
All imaging was performed using the 3-Tesla Siemens Magnetom Trio Tim System (Siemens Medical Solutions, Inc., Iselin, NJ, USA) at the Korea University Brain Imaging Center. The structural brain images were taken with a high-resolution T1-weighted MP-RAGE (magnetization prepared rapid acquisition gradient echo) sequence (1900 ms repetition time, 2.6 ms echo time, 220 mm field of view, 256×256 matrix size, 176 coronal slices without gap, 1×1×1 mm3 voxels, 16° flip angle, number of excitations=1). A radiologist reviewed T1 and fluid-attenuated inversion-recovery (FLAIR) scans to exclude overt structural abnormalities in the brain from further analysis.
Brain parcellation
Automated brain parcellation was conducted using FreeSurfer (software version 7.4.1, http://surfer.nmr.mgh.harvard.edu). FreeSurfer was adopted in the current study because of its well-established accuracy and reliability for automated structural brain image analysis [23, 24] and higher reproducibility compared with other methods [25]. The automated pipeline comprised motion artifact correction, removal of non-brain tissue, Talairach transformation, tissue segmentation, tessellation of the gray matter–white matter boundary, correction for topological defects, intensity normalization, surface deformation, and parcellation into anatomical regions. Visual inspection for brainstem segmentation accuracy was also performed. Total intracranial volume (TIV) was calculated with FreeSurfer and used as a covariate to correct for interindividual differences in brain size. Following the guidelines used by FreeSurfer, all participant data were processed on a single Linux workstation (Ubuntu 18.04, dual E5-2687W 3.10 GHz processor, 128 GB memory) to prevent unexpected data irregularities.
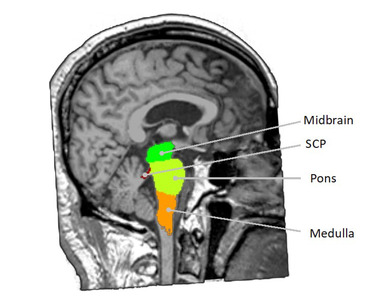
Brainstem volume analysis
A robust Bayesian inference algorithm was adopted to detect local variation within the brainstem subfield to segment and calculate the volumes of each subarea. The Bayesian segmentation approach based on a probabilistic atlas allows for the volumes of the medulla, pons, midbrain, and superior cerebellar peduncle to be calculated automatically [26].
Statistical analysis
Statistical analyses were performed using R software, version 4.1.2 (https://www.r-project.org). First, independent t-tests were performed to examine the age, education and TIV differences between groups. Second, an independent samples t-test was conducted to assess the between-group differences in the four substructures of the brainstem. A multivariate analysis of covariance (MANCOVA) was performed using the R jmv package (version 2.4.11) to assess volumetric differences while controlling for TIV. Bonferroni correction was applied to correct for multiple comparisons of four subregions [27]. The analysis included group (panic, control) as the between-subject independent factor, the volume of the regions of interest in four brainstem structures (medulla, pons, midbrain, and superior cerebellar peduncle volumes) as the dependent variable, and TIV as the covariate.
RESULTS
Demographic and clinical variables
A total of twenty-one PD patients and age-gender-education–matched healthy controls were recruited to participate in this study. There were no significant differences in age, gender, or education between the control group and the PD group (Table 1). In the PD group, the mean PDSS score was 9.01±4.74, with a cutoff score of 8 serving as an indicator for identifying patients with PD [19]. The mean HAM-A score was 15.62±10.39, with scores within the range of 15 to 23 indicating moderate anxiety [28]. The mean STAI-S and STAI-T scores were 44.33±7.02 and 42.90±9.65, respectively. For these scales, designed to assess current anxiety symptoms and propensity toward anxiety, respectively, a score of 40 is the established cutoff point [29-31]. The mean ASI-R score was 51.10±17.95. In a study of 267 patients diagnosed with PD, the mean ASI-R score was 47.41, demonstrating a notable association with functional impairment [32].
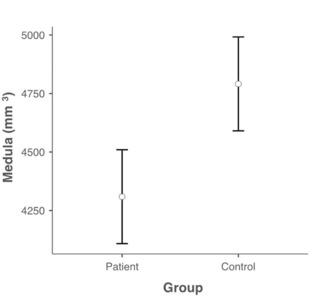
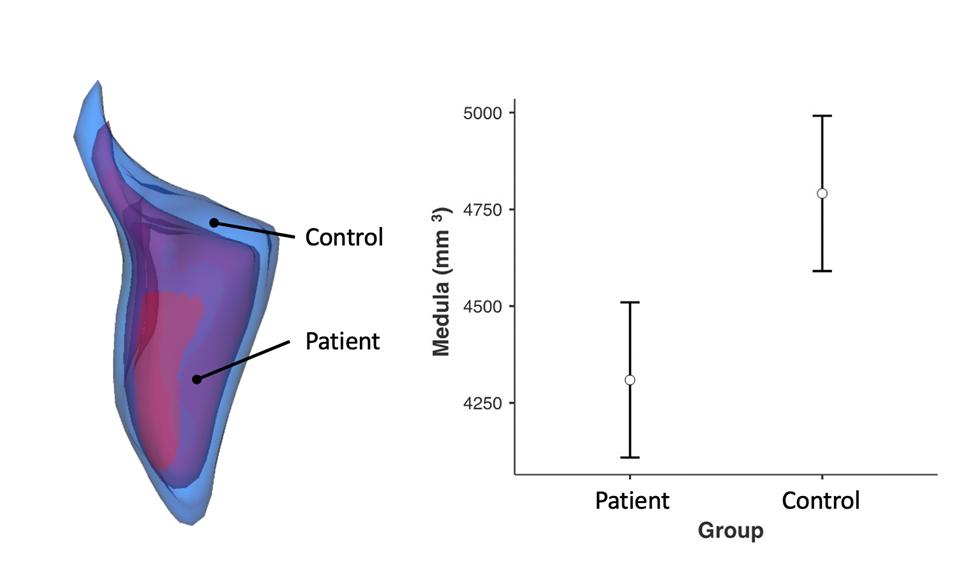
Brainstem structure
When compared with the control group, individuals diagnosed with PD were found to have significantly smaller medulla oblongata volumes (Fig. 1, 2). However, no statistically significant differences were observed in other brainstem structures (Table 2). A MANCOVA was conducted to further control for the effect of TIV. In this analysis, the medulla oblongata was still found to have a significantly lower volume in individuals diagnosed with PD (Table 3) after Bonferroni correction (p<0.011, Bonferroni-adjusted threshold of 0.05=0.0125).
DISCUSSION
The major finding of our study was that individuals with PD had significantly smaller average volumes of the medulla compared to healthy participants. This finding remained significant after controlling for variations in TIV. The medulla is associated with cardiovascular regulation and functions as an autonomic center. Sympathetic premotor neurons in the medulla influence sympathetic outflows via the descending efferent pathway. The C1 adrenergic neurons in the medulla regulate sympathetic vasomotor activity and function as a sympathoexcitatory response to stressors [6, 33-35]. The medulla receives signals from various regions, including the midbrain and the dorsal raphe nucleus, and plays a role in mediating automatic fear responses and receiving projections from PAG [36-40]. When activated, neurons in the PAG influence the 5-HT1A receptors in the rostral ventrolateral medulla (RVLM), which reduces sympathetic activity and lowers blood pressure. A study in cats demonstrated that injection of the 5-HT1A receptor activator 8-OH-DPAT into the RVLM resulted in a reduced sympathetic response. Neurons from the dorsal raphe nucleus, which are serotonergic, innervate the C1 adrenergic neurons, and influence sympathetic activity via 5-HT1A receptors. Accordingly, the RVLM can suppress stress-induced sympathetic responses by releasing 5-HT [34, 41-43]. Lactate infusion induces a panic response in the forebrain, limbic structures, and brainstem, activated via the dorsomedial hypothalamus/perifornical efferent pathway. The accompanying cardiovascular response can be attributed to activation in several brainstem areas. C1 and C2 adrenergic neurons, associated with autonomic regulation, respond to lactate. Similarly, C1 neurons, particularly in the medulla, can influence cardiovascular responses, and the nucleus of the solitary tract influences the baroreflex. Tachycardia occurs because lactate stimulates the parabrachial nucleus in the brainstem, which is responsible for respiratory control [44]. Furthermore, Yoshida et al. [45] found that, in the context of conditioned fear, neurons in the RVLM that synthesize prolactin-releasing peptides influence neuroendocrine responses in animals. The medulla is an area where 5-HT can function to prevent panic-associated cardiovascular responses, and dysfunction in the RVLM can lead to exaggerated panic symptoms [44, 46].
Few neuroimaging studies have focused on specific subregional volume alterations to brainstem structures in PD; however, alterations to these structures have been observed [47]. Fujiwara et al. [48] reported an increased dorsal midbrain volume, including the PAG, in patients compared to healthy controls, and these volume changes might reflect the severity. Gray matter volume has been measured using voxel-based morphometry, with increases noted in the midbrain and pons [49]. Another study demonstrated increased gray matter volume in the midbrain and rostral pons [50]. However, to our knowledge, no studies to date have investigated morphological changes in the medulla in the PD context. The current study showed that individuals with PD had significantly lower brain volume in the medulla relative to the control group. These results align with our understanding of the neurobiology related to panic attacks.
The present study has several limitations that should be acknowledged. First, the sample size is small, mainly because of the strict inclusion and exclusion criteria. Patients with PD often have comorbid psychiatric disorders; however, comorbid psychiatric conditions are known to be associated with structural abnormalities in the brain. We believe that the absence of a comorbid anxiety disorders may enhance the validity of this study by minimizing potential confounding factors that could have affected the structural data. Nevertheless, the generalizability of this study’s findings is inherently constrained by the limited sample size, which may not provide a comprehensive representation of the larger population. Second, the limited number of samples available made it impossible to analyze volume differences according to symptom severity. Finally, this study was limited by its cross-sectional design based on retrospective reports, which rendered temporal relationships and causative conclusions indiscernible. Therefore, subsequent investigations must engage in prospective study modalities to substantiate and expand upon the preliminary insights derived from this study. Future systematic research with a larger sample size is needed. In conclusion, structural abnormalities in the medulla may play a central role in the underlying pathophysiology of PD. The limited sample size in this study made it difficult to conduct further analysis to identify relationships between symptom severity and structure volume. Structural abnormalities in the amygdala and hippocampus have been suggested as potential biomarkers for PD; however, despite some limitations, our findings suggest the possibility of structural abnormalities in the medulla as another potential biomarker. Future studies could benefit from combining structural MRI with functional imaging techniques and neurotransmitter research [51].
ACKNOWLEDGEMENTS
This work was supported by a grant from Korea University (K2325951).
Figures
Tables
Demographic data and psychological scales
| Controls (n=21) | Patients (n=21) | df | T | p-value | |
|---|---|---|---|---|---|
| Agea) | 41.71 (12.14) | 39.29 (10.22) | 40.0 | 0.701 | 0.487 |
| Sex (male/female)b) | 12/9 | 12/9 | 1 | - | 1.000 |
| Education (years)a) | 14.0 (2.67) | 13.1 (3.25) | 40.0 | 1.089 | 0.283 |
| TIVa) | 1358 (159) | 1452 (126) | 40.0 | 2.130 | 0.039* |
| HAM-A | 17.67 (10.19) | - | - | - | |
| PDSS | 9.62 (4.61) | - | - | - | |
| ASI-R | 54.01 (41.83) | - | - | - | |
| STAI-S | 44.05 (7.28) | - | - | - | |
| STAI-T | 42.10 (9.44) | - | - | - |
ASI-R, Anxiety Sensitivity Index-Revised; PDSS, Panic Disorder Severity Scale; HAM-A, Hamilton Anxiety Rating Scale; STAI-S, State-Trait Anxiety Inventory-State; STAI-T, State-Trait Anxiety Inventory-Trait, TIV, Total Intracranial Volume. Data are presented as means (SD). a) independent samples t-test, b) Chi-square test * p<0.05.
The result of independent samples t-test of brainstem structures volume between PD patients and control group
| Controls (n=21) | Patients (n=21) | df | T | p-value | |
|---|---|---|---|---|---|
| Medulla | 4733.06 (467.29) | 4367.22 (474.73) | 40.0 | 2.517 | 0.016* |
| SCP | 274.55 (40.39) | 289.02 (59.83) | 40.0 | 0.919 | 0.364 |
| Midbrain | 6248.38 (633.08) | 6172.21 (464.26) | 40.0 | 0.445 | 0.659 |
| Pons | 14504.48 (1666.58) | 14337.99 (1407.40) | 40.0 | 0.350 | 0.728 |
| Whole brainstem | 25760.47 (2676.07) | 25166.45 (2193.95) | 40.0 | 0.787 | 0.436 |
SCP, superior cerebellar peduncle. Data are presented as means (SD). * p<0.05.
Summary of the multivariate analysis of covariance (MANCOVA) results
| Dependent variable | Sum of squares | df | Mean square | F | p-value | |
|---|---|---|---|---|---|---|
| Group | Medulla | 1410000 | 1 | 1410000 | 7.187 | 0.011* |
| Pons | 291057 | 1 | 291057 | 0.200 | 0.657 | |
| SCP | 2200 | 1 | 2200 | 0.850 | 0.362 | |
| Midbrain | 60921 | 1 | 60921 | 0.380 | 0.541 | |
| TIV | Medulla | 1250000 | 1 | 1250000 | 6.385 | 0.016 |
| Pons | 38500000 | 1 | 38500000 | 26.454 | <0.001 | |
| SCP | 3265 | 1 | 3265 | 1.261 | 0.268 | |
| Midbrain | 6070000 | 1 | 6070000 | 37.796 | <0.001 | |
| Residuals | Medulla | 7630000 | 39 | 195540 | ||
| Pons | 56700000 | 39 | 1450000 | |||
| SCP | 100951 | 39 | 2588 | |||
| Midbrain | 6260000 | 39 | 160509 |
SCP, superior cerebellar peduncle; TIV, total intracranial volume. * p<0.05.
References
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (DSM-5-TR). 5th ed. American Psychiatric Publishing, Inc., Washington, D.C.
- Asami T, Yoshida H, Takaishi M, Nakamura R, Yoshimi A, Whitford TJ, Hirayasu Y (2018) Thalamic shape and volume abnormalities in female patients with panic disorder. PLoS One 13:e0208152
- Gorman JM, Kent JM, Sullivan GM, Coplan JD (2000) Neuroanatomical hypothesis of panic disorder, revised. Am J Psychiatry 157:493-505
- LeDoux JE, Iwata J, Cicchetti P, Reis DJ (1988) Different projections of the central amygdaloid nucleus mediate autonomic and behavioral correlates of conditioned fear. J Neurosci 8:2517-2529
- Price JL, Amaral DG (1981) An autoradiographic study of the projections of the central nucleus of the monkey amygdala. J Neurosci 1:1242-1259
- Shouman K, Benarroch EE (2021) Central autonomic network. In: Autonomic nervous system and sleep: order and disorder (Chokroverty S, Cortelli P eds), pp 9-18. Springer, Cham
- McNaughton N, Corr PJ (2004) A two-dimensional neuropsychology of defense: fear/anxiety and defensive distance. Neurosci Biobehav Rev 28:285-305
- Graeff FG, Zangrossi H Jr (2010) The dual role of serotonin in defense and the mode of action of antidepressants on generalized anxiety and panic disorders. Cent Nerv Syst Agents Med Chem 10:207-217
- Sobanski T, Wagner G (2017) Functional neuroanatomy in panic disorder: status quo of the research. World J Psychiatry 7:12-33
- Perna G, Guerriero G, Brambilla P, Caldirola D (2014) Panic and the brainstem: clues from neuroimaging studies. CNS Neurol Disord Drug Targets 13:1049-1056
- Nash JR, Sargent PA, Rabiner EA, Hood SD, Argyropoulos SV, Potokar JP, Grasby PM, Nutt DJ (2008) Serotonin 5-HT1A receptor binding in people with panic disorder: positron emission tomography study. Br J Psychiatry 193:229-234
- Maron E, Kuikka JT, Shlik J, Vasar V, Vanninen E, Tiihonen J (2004) Reduced brain serotonin transporter binding in patients with panic disorder. Psychiatry Res 132:173-181
- Neumeister A, Bain E, Nugent AC, Carson RE, Bonne O, Luckenbaugh DA, Eckelman W, Herscovitch P, Charney DS, Drevets WC (2004) Reduced serotonin type 1A receptor binding in panic disorder. J Neurosci 24:589-591
- Boshuisen ML, Ter Horst GJ, Paans AM, Reinders AA, den Boer JA (2002) rCBF differences between panic disorder patients and control subjects during anticipatory anxiety and rest. Biol Psychiatry 52:126-135
- Sakai Y, Kumano H, Nishikawa M, Sakano Y, Kaiya H, Imabayashi E, Ohnishi T, Matsuda H, Yasuda A, Sato A, Diksic M, Kuboki T (2005) Cerebral glucose metabolism associated with a fear network in panic disorder. Neuroreport 16:927-931
- Oldfield RC (1971) The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 9:97-113
- American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders (DSM-IV). 4th ed. American Psychiatric Publishing, Inc., Washington, D.C.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59 Suppl 20:22-33; quiz 34-57
- Shear MK, Rucci P, Williams J, Frank E, Grochocinski V, Vander Bilt J, Houck P, Wang T (2001) Reliability and validity of the Panic Disorder Severity Scale: replication and extension. J Psychiatr Res 35:293-296
- Maier W, Buller R, Philipp M, Heuser I (1988) The Hamilton Anxiety Scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord 14:61-68
- Spielberger CD, Gonzalez-Reigosa F, Martinez-Urrutia A, Natalicio LF, Natalicio DS (1971) The state-trait anxiety inventory. Interam J Psychol 5:145-158
- Lim YJ, Yu BH, Kim JH (2007) Korean Anxiety Sensitivity Index-Revised: its factor structure, reliability, and validity in clinical and nonclinical samples. Depress Anxiety 24:331-341
- Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, van der Kouwe A, Killiany R, Kennedy D, Klaveness S, Montillo A, Makris N, Rosen B, Dale AM (2002) Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 33:341-355
- Fischl B (2012) FreeSurfer. Neuroimage 62:774-781
- Velasco-Annis C, Akhondi-Asl A, Stamm A, Warfield SK (2018) Reproducibility of brain MRI segmentation algorithms: empirical comparison of local MAP PSTAPLE, FreeSurfer, and FSL-FIRST. J Neuroimaging 28:162-172
- Iglesias JE, Van Leemput K, Bhatt P, Casillas C, Dutt S, Schuff N, Truran-Sacrey D, Boxer A, Fischl B; Alzheimer's Disease Neuroimaging Initiative (2015) Bayesian segmentation of brainstem structures in MRI. Neuroimage 113:184-195
- Bonferroni CE (1936) Teoria statistica delle classi e calcolo delle probabilità. Pubblicazioni del R. Istituto superiore di scienze economiche e commerciali di Firenze 8, pp 3-62. Seeber, Firenze
- Matza LS, Morlock R, Sexton C, Malley K, Feltner D (2010) Identifying HAM-A cutoffs for mild, moderate, and severe generalized anxiety disorder. Int J Methods Psychiatr Res 19:223-232
- Emons WH, Habibović M, Pedersen SS (2019) Prevalence of anxiety in patients with an implantable cardioverter defibrillator: measurement equivalence of the HADS-A and the STAI-S. Qual Life Res 28:3107-3116
- Wiglusz MS, Landowski J, Cubała WJ (2019) Psychometric properties and diagnostic utility of the State-Trait Anxiety Inventory in epilepsy with and without comorbid anxiety disorder. Epilepsy Behav 92:221-225
- Julian LJ (2011) Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken) 63(Suppl 11):S467-S472
- Kim HJ, Kim JE, Lee SH (2021) Functional impairment in patients with panic disorder. Psychiatry Investig 18:434-442
- Madden CJ, Ito S, Rinaman L, Wiley RG, Sved AF (1999) Lesions of the C1 catecholaminergic neurons of the ventrolateral medulla in rats using anti-DbetaH-saporin. Am J Physiol 277:R1063-R1075
- Johnson PL, Lightman SL, Lowry CA (2004) A functional subset of serotonergic neurons in the rat ventrolateral periaqueductal gray implicated in the inhibition of sympathoexcitation and panic. Ann N Y Acad Sci 1018:58-64
- Lovick TA (1993) The periaqueductal gray-rostral medulla connection in the defence reaction: efferent pathways and descending control mechanisms. Behav Brain Res 58:19-25
- Abols IA, Basbaum AI (1981) Afferent connections of the rostral medulla of the cat: a neural substrate for midbrain-medullary interactions in the modulation of pain. J Comp Neurol 201:285-297
- Selionov VA, Shik ML (1984) Medullary locomotor strip and column in the cat. Neuroscience 13:1267-1278
- Garcia-Rill E, Skinner RD (1987) The mesencephalic locomotor region. I. Activation of a medullary projection site. Brain Res 411:1-12
- Sewards TV, Sewards MA (2002) Fear and power-dominance drive motivation: neural representations and pathways mediating sensory and mnemonic inputs, and outputs to premotor structures. Neurosci Biobehav Rev 26:553-579
- Bago M, Marson L, Dean C (2002) Serotonergic projections to the rostroventrolateral medulla from midbrain and raphe nuclei. Brain Res 945:249-258
- Helke CJ, Capuano S, Tran N, Zhuo H (1997) Immunocytochemical studies of the 5-HT(1A) receptor in ventral medullaryneurons that project to the intermediolateral cell column and contain serotonin or tyrosine hydroxylase immunoreactivity. J Comp Neurol 379:261-270
- Bago M, Sprtel BM, Dean C (1999) Modulation of sympathetic nerve activity by microinjection of the 5-HT1A receptor agonist 8-OH-DPAT into the rostroventrolateral medulla. J Auton Nerv Syst 76:127-134
- Bago M, Dean C (2001) Sympathoinhibition from ventrolateral periaqueductal gray mediated by 5-HT(1A) receptors in the RVLM. Am J Physiol Regul Integr Comp Physiol 280:R976-R984
- Johnson PL, Truitt WA, Fitz SD, Lowry CA, Shekhar A (2008) Neural pathways underlying lactate-induced panic. Neuropsychopharmacology 33:2093-2107
- Yoshida M, Takayanagi Y, Onaka T (2014) The medial amygdala-medullary PrRP-synthesizing neuron pathway mediates neuroendocrine responses to contextual conditioned fear in male rodents. Endocrinology 155:2996-3004
- Johnson P, Lowry C, Truitt W, Shekhar A (2008) Disruption of GABAergic tone in the dorsomedial hypothalamus attenuates responses in a subset of serotonergic neurons in the dorsal raphe nucleus following lactate-induced panic. J Psychopharmacol 22:642-652
- Del Casale A, Serata D, Rapinesi C, Kotzalidis GD, Angeletti G, Tatarelli R, Ferracuti S, Girardi P (2013) Structural neuroimaging in patients with panic disorder: findings and limitations of recent studies. Psychiatr Danub 25:108-114
- Fujiwara A, Yoshida T, Otsuka T, Hayano F, Asami T, Narita H, Nakamura M, Inoue T, Hirayasu Y (2011) Midbrain volume increase in patients with panic disorder. Psychiatry Clin Neurosci 65:365-373
- Uchida RR, Del-Ben CM, Busatto GF, Duran FL, Guimarães FS, Crippa JA, Araújo D, Santos AC, Graeff FG (2008) Regional gray matter abnormalities in panic disorder: a voxel-based morphometry study. Psychiatry Res 163:21-29
- Protopopescu X, Pan H, Tuescher O, Cloitre M, Goldstein M, Engelien A, Yang Y, Gorman J, LeDoux J, Stern E, Silbersweig D (2006) Increased brainstem volume in panic disorder: a voxel-based morphometric study. Neuroreport 17:361-363
- Cosci F, Mansueto G (2019) Biological and clinical markers in panic disorder. Psychiatry Investig 16:27-36